I realize some readers won’t have read the post I’m correcting, and won’t be interested, so first here are some topics I plan to write about in the coming months:
Zuranolone, a new GABA-ergic medication that recently received FDA approval for postpartum depression. We’re in the process of submitting a viewpoint article critiquing the approval, but I will plan to write about this here, hopefully once it is published.
Hopefully my final post about the maternal RSV vaccine, this letter to the editor we wrote was published in the NEJM, which finally let us see at least one important piece of all-cause data. Here’s the key quote,
“Modest efficacy was observed against hospitalization for lower respiratory tract illness of any cause (vaccine efficacy, 29%; 95% CI, −2 to 51). However, this finding could have been influenced by the unusual epidemiologic circumstances during the Covid-19 pandemic, in which RSV-associated lower respiratory tract illnesses constituted 22% of bronchiolitis cases among infants younger than 1 year of age as compared with 50 to 80% of cases in prepandemic studies.”
I would argue that an unusual seasonality doesn’t relieve the sponsor of needing to show vaccine efficacy against all-cause LRTI hospitalization.
Colchicine for prevention of cardiovascular disease. Looking forward to reading about this one, haven’t read any of the studies yet.
There will be plenty more, I’m always happy to take any suggestions for topics. Now onto the correction.
This correction is about an old post from October 2022. I always welcome criticism and will obviously make mistakes occasionally when I write. Where these are brought to my attention I will issue corrections. In the post I wrote about the relative risk of hospitalization in adolescent/young adult men from the primary covid vaccine series and natural infection from covid.
The relevant CDC data linked is here. One mistake I made was citing the peak weekly rate of covid hospitalization of 2.1 per 100,000, instead of the cumulative rate of 49.9 per 100,000. This was sloppy, and I will be more careful in the future. That being said, I don’t think it impacts the core claim, being this:
The full primary vaccine series (almost all from 2nd shot) carried a small, but likely higher risk of hospitalization as compared to natural infection in healthy adolescent/young adult males.
Note: Even if they are just within the same ballpark, the cost/benefit is iffy
Let’s walk through the data and discuss it the way I should have the first time. The cumulative rate throughout this study period was 49.9 per 100,000. According to the CDC document, about 55% of these hospitalizations were thought to be “from covid”, meaning the other 45% were likely incidentally positive on admission, or hospitalized “with” covid. If we focus on “for covid”, that gives us ~27.5 per 100,000.
Edit: I saw the clear error previously and caught another one when I went back to read the study. I previously wrote about the difficulty with estimating the hospitalization rate with respect to total infections, but that is actually not relevant in this case, given they used population numbers. The lesson learned (twice over) is to avoid sharing something without looking back over it multiple times. A night’s sleep is great for catching things you missed. This is a good example of why I now try to avoid a lot of this observational stuff where there are endless studies with wide ranges in estimates of whatever you look for (hospitalization 2/2 covid vs. vaccine myocarditis, etc.). Sticking with drug approvals and clinical trial analysis is much less noisy.
This study is a good example of how much these estimates vary, “The highest incidence of myocarditis ranged from 8.1-39 cases per 100,000 persons (or doses) in studies using four stratifiers. Six studies reported an incidence greater than 15 cases per 100,000 persons (or doses) in males aged 12-24 after dose 2 of an mRNA-based vaccine.”
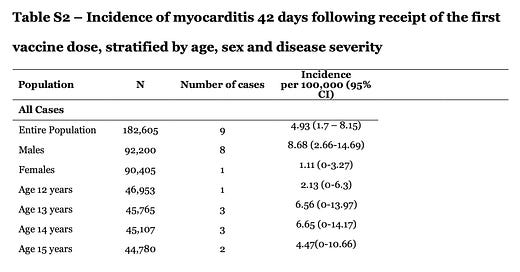
Here is the screenshot from the supplementary appendix of the Pfizer vaccine risk study I had originally been looking at, linked here.
Another relevant variable in the cost-benefit here is baseline health status. This is from the CDC data, speaking of those hospitalized adolescents, “Overall, 70.6% had one or more underlying medical conditions, the most common of which were obesity (35.8%), chronic lung disease, including asthma (30.9%), and neurologic disorders (14.2%).” This is another reason to take into account risk stratification in decision making around these shots.
Always happy to hear thoughts, critiques, and any topics people are interested in.